A collection of stories from people across the country explaining in their own words living with the long-term complications of COVID-19. They are part of an 80,000+ member support group on Facebook called Survivor Corps
27 photos
1/27

I was a healthy 46-year-old woman until 99 days ago when COVID took over my entire body. Serious GI issues are too numerous to list, and I am in constant pain. I have hearing loss, my vision is blurred, a horrible rash, unexplained bruising. I have neuropathy in my hands and feet and constant tremors. My hair is falling out, I can't eat and I'm constantly dehydrated. I am dizzy, disoriented and exhausted and have lost an extreme amount of weight. Constant anxiety My immune system is completely depleted and I cannot fight this horrible virus. Numerous doctors, ER visits, procedures, and specialists, with more to come. This virus is paralyzing me and I don't know if these symptoms are reversible or if the damage is permanent. Not knowing when and if I will ever improve is my biggest fear.
2/27

My name is Gail Pesses. I live in Metairie, LA, a suburb of New Orleans. After finding out that COVID was here during Mardi Gras, my adult children, who had both come in from out of state for one of our best Mardi Gras Days ever, and I counted off the weeks following. When all 3 of us were still healthy 4 months later, we thought we were home free, but then I got sick in early April with chills followed by constant diarrhea. No fever. No cough. I called my doctor who had me tested for COVID. Negative. I developed shooting pains on my side, sharp constant pain in both legs, more diarrhea, shortness of breath, complete exhaustion and pressure on my chest (like an elephant was sitting on it.) A second COVID test also came out negative. I was pretty sick. There were several nights I was truly scared of dying. Yet my oxygen levels were good, so I resisted going to the ER. I feared getting sicker there or ending up on a ventilator. Friends could not believe I was still sick. Finally at the beginning of May, I heard that the doctors at my doctor’s hospital were going to begin seeing patients in person. I knew I was getting worse and had to see a doctor. I was lucky to get an appt, the last appt for the next day with a different doctor. She sat with me, listened to all I had been through so far, listened to my lungs, chest, etc and fully examined me. (She was the first/ only dr to tell me that the Covid tests have a 30% false negative rate).She immediately sent me for more blood work, a chest x-ray, a cat scan of my chest and an ultrasound of my leg. She called me the same day with the results of all the tests. I had atypical pneumonia and my liver and pancreas were not functioning as well as they should. There were no blood clots in my legs. She prescribed medication for the pneumonia and warned me that I would be exhausted for the next 6 weeks. During the next 6 weeks, the chest pressure continued while the pain slowly receded. She sent me protonix and an inhaler which took 2 weeks to help. After 3 months, my constant diarrhea gave me a break for a day or 2. A new pattern started with no diarrhea for 1-2 days, then back to square 1. Then I was ok for 3-4 days, then back. As of 2 weeks ago, the diarrhea has been gone, only coming back 2 different days. I am still exhausted and have to pace myself daily so as not to overdo it.
Besides the obvious fears and frustrations of dealing with a new virus that so little is know about, it has been difficult to explain my “flavor” or it. I never ran fever( rarely do), did not have the sore throat or terrible cough identified initially as the reliable symptoms and my tests were negative. The symptoms I did have were not well documented until just a few weeks ago. Few people know how the virus really works and that it can last for months.
3/27

I am a 30 year old single mother in Boca Raton, Florida. I was a firefighter / paramedic at the time of infection. I am on day 130. I have a collapsed lung and have never been hospitalized, and have experienced around 70 symptoms. I feel like an absent parent because I can't do things that I used to do with my son. I can't even do basic housework or walk my dog more than 100 feet. I have not been able to receive any kind of medical care due to lack of confidence and problems with insurance and workers compensation. I created a survey with over 1,500 responses for those like me who want to educate and raise awareness about the long distance experience. The world needs to be aware that it is not a cold or flu.
4/27

Diagnosed and put into isolation for 8 weeks in mid-March, 2020. Doctors, nurses and I read CDC guidelines, WHO info, etc. together as at that time, they had little to go on. Still fighting some symptoms, although I finally got a test recently and showed negative, which I was told didn't mean a lot as the tests have problems with false negatives. Have definitely improved over 4 months ago, but far from being back to normal. Still have to lie down for a while after I shower, and my energy levels are junk. Some better days, some bad. No predictable pattern. Being in isolation for 8 weeks, apart from my husband and dogs, was challenging. I created a "stained glass window" coloring page that I colored in a bit every day and a program I followed to keep my spirits up, designed in chats with doctors and nurses.
5/27

Jessica Standifird
My name is Jessica and I've been sick since March 11th. I am on an upswing, but overall it's been a two steps forward, three back journey. You feel better, nearly human again, for a few days and then bam, you're fatigued and too weak to do anything. Or your fever comes back. Or your symptoms change from respiratory issues to GI issues. It's like being gaslighted by a disease- so many seemingly unconnected symptoms. I've had skin abnormalities (rash, odd scarring and reactions), fevers as high as 104.1, conjunctivitis in the eye, the symptoms listed above, and mouth ulcers, to name a few. There is so much to say. I lived in San Diego before moving to Portland, OR 8 years ago.
6/27

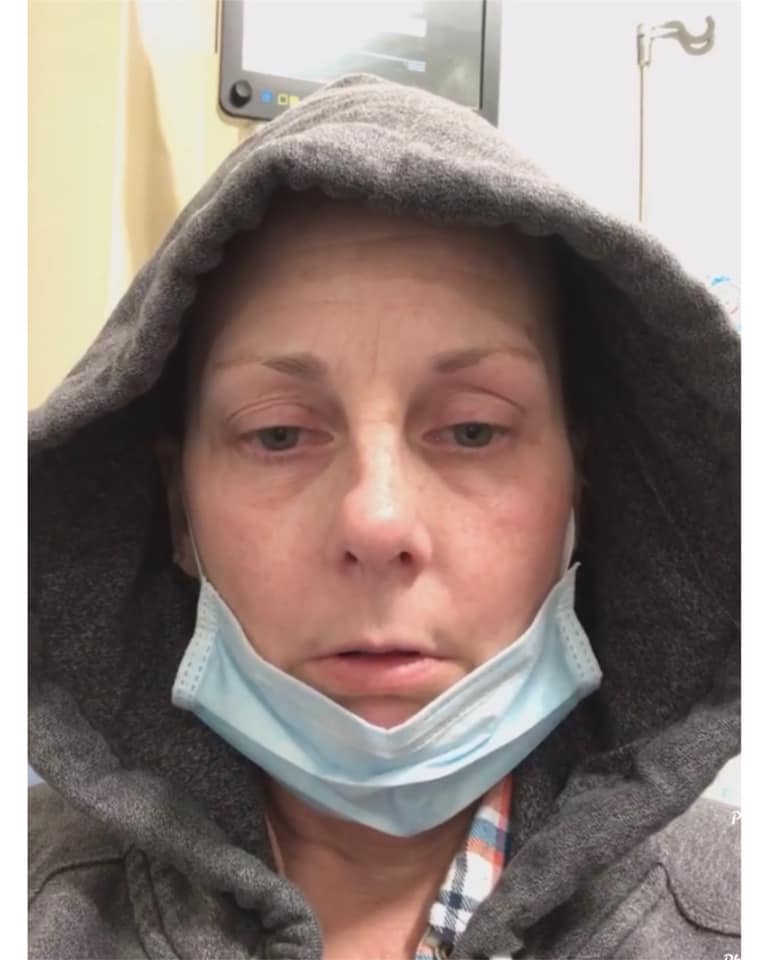
I was in the hospital from March 24 to April 5 and 4 months later I still have tachycardia, hair loss, fatigue and many other persistent symptoms. I was in critical condition, and my body and mind have not yet recovered. At first she had an autoimmune disease acquired as a survivor of September 11. Contrary to what skeptics say, it's not just about the death toll, but about the suffering of survivors.
7/27
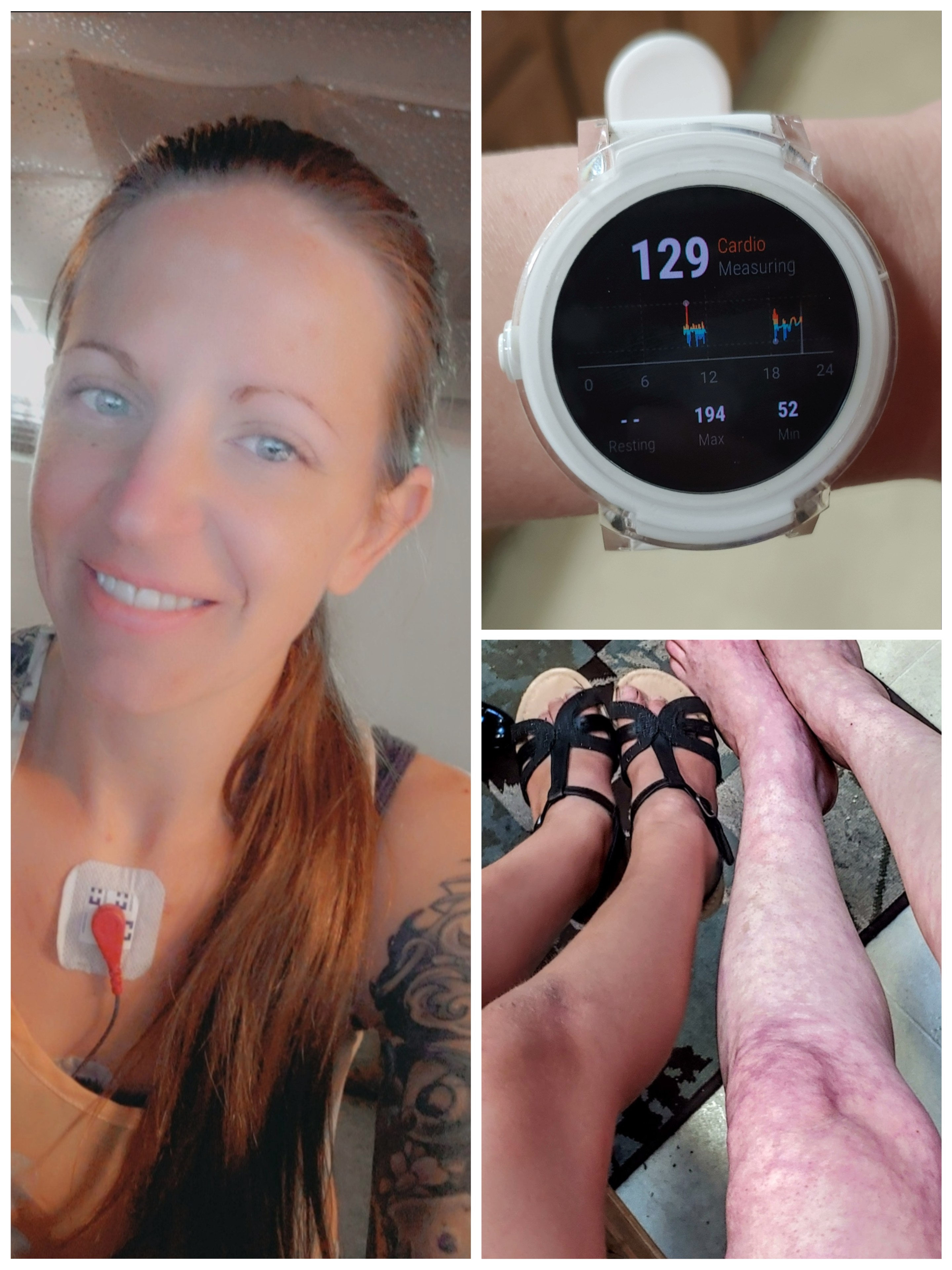
Mid March, exactly 5 days after having contact with someone who traveled to the epicenter of this virus, I developed a low grade fever and shortness of breath. Speaking felt like I just ran a marathon. I was tested 1 day later as a healthcare worker. Negative results. Fast forward 116 days later and I am still experiencing daily fevers and shortness of breath. I've added to that list tachycardia, livedo reticularis (those lovely legs below), headaches, dizziness, fatigue, and brain fog.
I've forgotten my social security number at times. I can't sleep, but I'm exhausted. I'm not sprinting down the street to get my heart rate that high, I stand up. My new normal heart rate at rest is usually 110-120 and if I stand up it rises as high as 195 bpm. No answers, no magic cure, no provider I've spoken to who is aware of the symptoms my new covid survivor family is going thru. But we're resilient. We got this, together. #ThisVirusWontBreakMe
8/27

Prior to COVID I was a healthy 46-year-old marathon runner. 107 days later I still continue to fight off this horrific rollercoaster of a virus. I'm fearful that my body will never recover. Rushed to the ER yesterday by my doctor for a abnormal EKG and blood so thick that they couldn't draw it to run tests. I'm now on blood thinners to reduce my chances of clots and ease the tension in my heart. This virus is relentless and does not only affect those with underlying issues. I'm hopeful that I will one day run again, but for now I'm just happy that I can take my dog for a 10 minute walk.
9/27

Covid ruined my life, but I am a survivor. I’ve lived through my sons drug addiction and the loss of 2 husbands. I will survive this and come out on the other side!
10/27

He was very close to death. Now he is at home and is better, but he has persistent problems. Unable to sleep, he has PTSD, rapid heart rate, RLS, pain and numbness in the extremities, joint pain, and loss of voice. This virus is not a government hoax or conspiracy, but a real virus that affects real people.
11/27

March 25th -Covid 19 hit me like a freight train! 4x's in and out of hospitals, Pulmonary embolisms, blood clots in lungs, bilateral pneumonia, tachycardia, macular hole in my retina, etc. The list goes on and on, but here I stand today 118 days later and living life! As I said from day 1, dig deep and fight the fight! It takes mental toughness and determination to win this war and I refuse to go down! Find the silver lining in your life and go after it!
JerseyStrong
12/27

I tested positive March 19th and still experiencing loss of smell. Once I realized my loss of smell is an extensive effect of COVID I installed additional smoke and carbon monoxide detectors as a safety precaution and to ease my paranoia. Last week, my family and I went to bed and sometime during the night I was woke out of my sleep by God warning me that something wasn't right in my house. I laid in my bed a few minutes afterwards and began to smell a funny odor but I wasn't sure because I hadn't been able to smell for a long time. I got out of bed and went to the kitchen and smelled a strong scent which was gas escaping from my stove, one of the pilots was on high. I turned everything off and checked the carbon monoxide detective and discovered I never activated the detector. It's activated now! Thank God nothing serious happened to me and my family.
As of result of this I'm trying Aromatherapy with smelling coffee brewing, coffee beans. I've tried Eucalyptus a few times it opens my nose and I'm able to smell for a short period of time but it goes back to limited sense of smell. I never imagine not being able to smell as normal but I'm hopeful this will pass soon.
13/27
This was day one in the ER on March 28th. I was waiting for oxygen. Over 100 days later I now have a blood clot in my left leg. The diagnosis is Small Vein Thrombosis. The clot is not in danger of breaking off, but has to be monitored closely and I now have to take aspirin and prescription Folic Acid for it. I have Right Bundle Branch Blockage which showed up on a post Covid EKG. My neuropathy has gotten worse since Covid, and I now thump when I walk. Thickening on my right lung, hair is still falling out, brain fog, severe anxiety, and blurred vision. Eye doctor appointment is next week. I was not recovered after 14 days. It took 47 days before I was able to come out of isolation.
14/27

I became ill in late Feb-early March. Late Feb. had gastrointestinal issues. March 3rd went to urgent care with pressure in chest & shortness of breath. In urgent care became very difficult to breathe and Oxygen levels went down. They sent me to ER in an ambulance. Treated with oxygen and intravenous anti-inflammatory/pain reducer for 8 hours & released. March to mid-July experienced, chest pain/pressure (like punched in middle of chest), shortness of breath, bouts of low oxygen (low 90's -high 80's), difficulty talking due to SOB, sweats, respiratory infection/sinusitis, headaches, diarrhea, fatigue, weakness, vertigo, loss of taste & smell. I now have pattern of ground glass opacities in my lungs and lung damage that my pulmonologist is unsure is reversible. I also have nerve damage in the nerves along my upper gums from having the respiratory infection for 4 1/2 months. This feels like having several toothaches at the same time. This, hopefully is reversible with time. The last several days, I have struggled with Bradycardia, increased chest pressure and SOB-struggling to talk again - due to SOB. Had this several times with COVID-19 - scared, confused and really want to get better!!!
15/27

I am a Doctor in NYC and came down with the Coronavirus on March 23, 2020. I was not well for 2-3 weeks but many of the symptoms lingered up until now.
My initial symptoms on March 23 was severe dysentery/diarrhea (15-20 bouts a day) and so I dropped 23 pounds, followed by fever, night sweats, shortness of breath, mild cough, rhonchi and crackles in my left lung field (using a stethoscope I could hear it), my Oxygen level using a Pulse Oximeter fell to 90 and that is why I had shortness of breath, extreme fatigue-(tired beyond words), extremely cold feet and hands, muscle/bone aches and pains, hair loss, lost my sense of smell and taste. I experienced very vivid dreams.
I always take showers every night and a few times I showered while I had Covid19, I almost passed out in the shower as I developed nausea.
My doctor wanted to admit me to the hospital but I knew what was going on in the hospitals and thought I would do better by staying at home under isolation and taking medication at home. I took Zithromax (ZPak) for 5 days and started to improve but was still very weak and lethargic and then continued on another Zithromax course for 5 days. I took these daily: 2 multivitamins, Vitamin B Complex, Zinc and Vitamin D 50,000 units (1 pill per week). I am also on Singulair for asthma (as I served as a doctor at Ground Zero after 9-11) so I took 1 pill every night. I took baby aspirin to reduce my fevers and take away the excruciating muscle and bone pains. I also did deep breathing exercises to get air into my lungs. I also had my son James (while he wore a mask and I wore one too) use a Theragun everyday on my entire back/lungs fields to use vibratory motions to keep everything flowing. I quarantined in my bedroom for 3 weeks. I relapsed when I had cleared CDC guidelines and I did 8 charity outreaches in one day, I developed fever and chills that night so I started a 3rd Zithromax (Z-ZPak).
I still had cold feet and hands and diarrhea into April and May, so I started Levaquin 750mg for 7 days which resolved the cold extremities.
I was tested for Covid with the nasopharyngeal swab and was positive.
I went for a venipuncture in May and tested positive for the antibodies. I started the paperwork to schedule and donate my plasma. I still have fatigue and hair loss since getting Covid19.
16/27
I first felt sick the night of March 15 th with a very slight fever (100) and asthmatic cough. The next day I was coughing more. Called my doctor’s office and they said I should be given a test because of my asthma and to call the northwell walk in. I called, was asked a bunch of questions, and told I didn’t qualify. By the next day, I felt it was more like a sinus infection. By the time I sat down to eat my corned beef and cabbage for St. Paddy’s Day, my taste was off. By the next morning, I couldn’t smell my coffee. I had no smell or taste at all. I called my doctor. He put me on prednisone. This was Friday the 20th, my head was so foggy and I’ve never lost my smell and taste before. The next day I felt worse and went to city md and was given amoxicillin for the sinus infection. Monday the 23rd, I called my doctor again and he switched me to Z-pack and gave me a second dose of prednisone. I had bad asthmatic cough all week and never got my smell or taste back. On March 27th, I got an email from Excel urgent care saying they had COVID tests. I called them. It was late. I told them my ordeal. The receptionist said I sound like qualify and to come down and call when I parked. They had me wear a mask and gloves and went right into a room. The nurse immediately gave me a test. The physicians assistant John saw me. He said my lungs were rattling badly and I needed an X-ray. I cruelly laughed and said it was my asthma. He said he would call me if the X-ray was positive. They were closing soon so I expected the call the next day. I got home and my phone rang almost immediately. He said i had the beginning of pneumonia and he thinks it’s Covid. The results would be a few days for the COVID test. He changed my antibiotic to cefdinir which i started the next day. I felt like I got hit by a bus by Saturday. I couldn’t eat and I couldn’t move. That Sunday, they called to tell me I was positive for COVID. I had the nebulizer at home, so I battled this beast by using it, resting up and drinking lots of water. The fatigue was crazy for a few days, along with headache and asthmatic cough. No fevers.
I retested on Good Friday April 10th and I was still positive! Retested again April 30th and was finally negative. I had another test to truly confirm.
I am currently dealing with asthmatic bronchitis. I was just put on more prednisone, steroid inhaler, nebulizer and Z-pack. The doctor said I’ll be on meds for months. I’m unable to workout. I’m usually a fitness junkie. Those with asthma should know, it’s going to take time and go easy on yourself.
Side note- I have 3 girls, husband and aunt and I’m the only confirmed case. My youngest is still nursing and I believe she got my antibodies as she has never been sick. I’ve been donating plasma. I’ve had some good runs with no bad flare ups right now it’s bad.
17/27

My name is Sarah & I live in Greenlawn, NY. I started feeling ill in April with loss of sense of smell/taste, fatigue, head ache/sinus pressure and ear pains. I tested positive on the 24th of April and quarantined for 3 weeks in my bedroom to avoid infecting my parents. My sense of smell/taste slowly came back and the other symptoms became manageable when my chest started to hurt. A dull pain that turned very quickly into stabbing spreading pains throughout my left side. This pain occurred every night for another month. I packed a hospital bag and wrote all of my personal info down in case I was rushed to the hospital. After several weeks, I went to the hospital after one night I thought my heart felt like it was going to explode. They ran every test on me - bloodwork, CT scan, MRI, echocardiogram. Nothing explained the pains I was having. After the hospital visit and 4 other Dr. appointments, I went to see a cardiologist and he stated it was simply a residual effect of COVID-19.
18/27

My first war with COVID-19 was 47 days, 45 of those with a fever and a wide array of symptoms that include bumps, COVID cough, low BP, nausea, vomiting, hair loss, tachycardia, muscle pain, extreme fatigue and headaches. Two times I was hospitalized and was probably five minutes from a ventilator.
I recovered, well I thought I did, and ultimately got sick again. Here I am in the second week of flare or post-viral symptoms with pneumonia, bumps, and every single symptom all over again.
19/27

I pulled out this blank diary the day after I was notified of my positive COVID test. I put the sticker on it to encourage me (you’ve got this!). I use it to track my symptoms, thoughts, and anything I learn to help me make good decisions about improving my health. I thought it had way too many pages, but 61 days later, I’m a COVID long hauler and this little journal is one of my lifelines in my recovery. Not quite running out of pages, but it is getting full. Also, I realized weeks into this that “You Got This” could also mean – you got this – this being COVID! You have to find humor in this craziness!
20/27

Diagnosed April 1, but it was no joke! Still experiencing episodic loss of taste and smell, hair loss/thinning, heart racing intermittently with minimal activity, elevated BP, bouts of fatigue. I have so much to be thankful for, so I’m not complaining.
21/27

I was sick with COVID in March, spent 16 days in the hospital, 12 days in ICU intubated. I got discharged in April 6, went back to my full-time job on May 24. I am for the most part doing great having survived and lived. My lasting symptoms include soreness on my left leg, shortness of breath that just comes on out of the blue, bad migraine and unexplained itchiness with welts and hives all over the body. I had lab draws done for blood clots and X-rays for the leg and it was normal. I had x-rays done post hospitalization and it is clear. My migraine feels very intense and much more debilitating. The hives and welts come sporadically, very itchy and is totally driving me insane. Although I am grateful to be COVID-free these lingering symptoms still affect me so much everyday. I try to move on far, far away from COVID but these lingering symptoms seem to not want me to move on.
22/27

COVID hit me mid-March. I was quarantined for eight weeks. For the first week, I had severe rib cage and chest pains. It felt like my rib cage was in a vice grip and someone was stepping on my chest at the same time. I had insomnia, fever, hallucinations, tingling and numbing all over my body, especially my legs and arms. The headaches were massive which I attributed to my hallucinations and brain fog. And the continuous whole body malaise and fever rocked my body as well…
It progressed to throat infection, diarrhea, conjunctivitis and hair loss.
I lost my sense of smell and taste on day five and it lasted for 9 nine weeks. The throat infection was so severe that I ended up in Urgent care and had to be on a z-pak.
I could barely swallow and when I did, it felt like shards of glass were going down my throat. I lost 18 pounds during this time.
I came out of quarantine on the ninth week, but the symptoms and complications are still riddling my body as we speak.
As I continued to recount my illness to a friend who is a nurse, she told me that the tingling and spasms on my arms, legs, fingers and toes were coming from poor oxygen saturation. The only way I was able to breathe is by flipping myself onto my stomach to relieve the pressure from my chest. Unbeknownst to me that doctors started to practice it later on on their patients.
I am on my 18th week and my intestinal issues and conjunctivitis came back. Muscle spasms, numbing and pain on my legs sometimes become severe that I have to take a couple days to recover.
I have insomnia again. My hair loss is still ongoing.
I have noticed my labored breathing and sometimes, my inability to get enough air in my lungs causes me to get lightheaded.
I have Graves disease, Crohn’s, fibromyalgia, rheumatoid arthritis and very asthmatic. My hands have been branded for about six weeks now. The darker the discoloration, the more my hands experience numbing and weakness.
I have gone back to being a fitness and wellness instructor, but it is a daily struggle.
I am a huge proponent of mask wearing... I believe in being selfless to show respect, love and kindness to my family, friends, and community… this should never be an issue. At the end of the day, we are all in this together and this too shall pass.
23/27

Hi, I am Marjorie and I have been riding the "Coronacoaster" for 16 straight weeks. My symptoms started mid-March and I was tested on April 4, told I was negative and sent home with information on viral infections. I proceeded to develop more COVID-19 symptoms that led to two additional trips to the emergency room and to me being sicker than I have ever been in my life.
After four lung X-rays, three EKG’S, three CT scans, one new primary Doctor later and visit to a lung specialist, it was determined that the negative COVID-19 test administered was a false negative… Next step for me, a scheduled Bronchoscopy which allows doctor to visualize scar tissue and nodules that have formed in my lungs.
24/27

Week 20, day 135 and still dealing with intermittent tachycardia, random oxygen drops, lingering shortness of breath, skin rash, ocassional GI issues, puffy, dry and scratchy eyes, nausea, little appetite, neurological symptoms like brain fog, forgetfulness, short term memory loss, blurry vision, insomnia, and numbness in my face. I now take blood thinners every day for the blood clot found in my lung in week 12.
I'm praying that we all eventually make it back to who we were before this.
25/27

Penn Valley, CA
I’m an RN, exposed at work on the front lines, and contracted covid 19 on March 24.
I started with a major headache, body aches, dizziness, swollen lymph nodes, and raging fatigue.
The hospital I worked for has been less than helpful, to say the least. They also fired me last month for still being ill. The just send me a bill for $12k to repay a bonus I was given last year.
I’m still unable to work. My disabled, retired military husband is taking care of me. At this point, 17 weeks of illness, I now use a twice daily steroid inhaler, a nebulizer when things are really bad, and have to take a beta blocker for my new high blood pressure and heart palpitations.
I pray I’m not permanently disabled, but it’s sure looking that way right now. I have no energy, no stamina, generalized muscle aches, tremors, short term memory problems, and too much sensory input is completely overwhelming.
If I can answer any further questions,
I’m more than happy to.
26/27

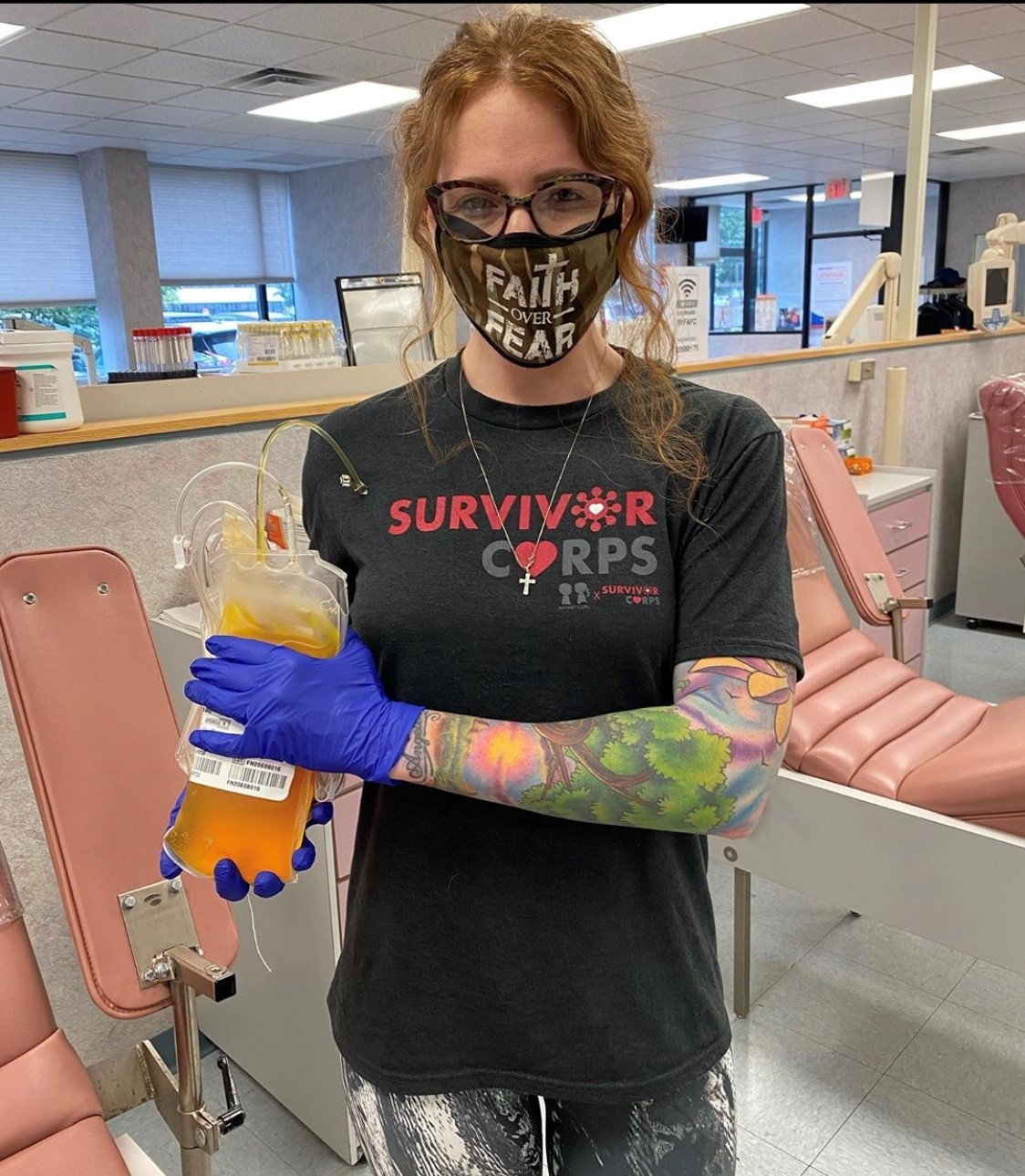
Symptoms persist at day 130 with GI issues, hair loss, brain fog, fatigue, loss of breath and chest pain. I am lucky enough to have antibodies and to have felt well enough to donate. The news around COVID should not only focus on the numbers but what life is like post-covid and how life altering symptoms can be!
27/27

I was diagnosed March 30, 2020 (this photo is from that day). I had a dry cough, the worst body aches I’ve ever felt, a low grade fever, chest pains, shortness of breath and did lose taste/smell. It was a roller coaster for about 2 weeks in isolation of my room. One day I was okay, the next I was not. I am thankful I was able to recover at home and do have antibodies now. But, here we are July 23, 2020 and I still have lingering symptoms. I have daily shortness of breath, and simple activities like walking up the steps drain me. After going up a single flight of stairs just yesterday, my HR rose to 178. I have rapid heart rate and chest pains as well. Prior to this I was a healthy 26-year-old with no prior conditions. While I am undergoing testing, the doctors just aren’t sure of any answers. I am technically “recovered,” but just don’t feel like me and am scared this is my new “normal.” Praying for everyone that we get better one day at a time.





